3D printed cell models are currently in the spotlight of medical research, thanks to the fact that 3D printing is starting to become a key element in the manufacture of native tissue replicas. Although significant progress has been made, there remain aspects requiring attention in order to obtain more realistic models that faithfully represent the in vivo environment. Much work remains to be done to produce effective materials that are printable, stable, have enhanced mechanical properties, and which are responsive to the desired stimuli, and that way enter the new era of 4D printing.
In a paper published by the Journal of Materials Chemistry B, CIC biomaGUNE’s Hybrid Biofunctional Materials research group has described how to produce an artery model with cyclic expansive properties and which is capable of mimicking the different physical forces and stress factors experienced by cells under physiological conditions. The described technique involves 3D printed tissue constructs that respond to stimuli, thereby providing a fourth dimension (4D); this offers a novel approach to producing dynamic biomodels.
The study features in the Emerging Investigators collection which highlights emerging researchers in materials chemistry who have been recommended by experts in their field for having conducted work with the potential to influence future directions in materials chemistry with applications in biology and medicine.
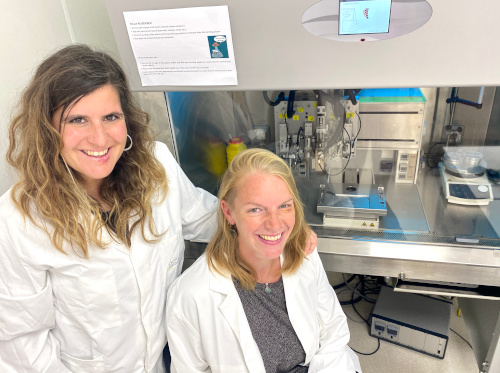
The research group focused on the development of printable hybrid materials that respond to external stimuli in order to reproduce forces occurring in the pulmonary arteries. “The results obtained so far point to the suitability of using 3D printing to generate 3D tissue models based on these hybrid bioinks comprising nanoparticles, hydrogels and cells of human origin,” explained the Ikerbasque Research Fellow Dorleta Jimenez de Aberasturi, who leads the group.
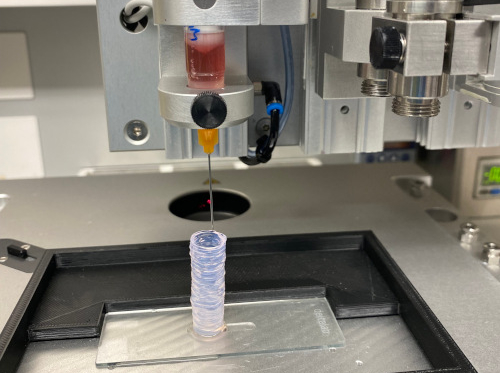
Arterial wall components are reproduced in three layers by means of 3D printing. “Polymers with gold nanoparticles that react to temperature changes are used to represent the outer tunica of the artery; smooth muscle cells embedded in an extracellular matrix represent the tunica media; and finally a monolayer of endothelial cells as the arterial tunica intima,” explained Dr Jiménez de Aberasturi, who was recently awarded a prestigious Ramón y Cajal Grant by the Spanish Ministry of Science and Innovation.
Dr Malou Henriksen-Lacey, a researcher at the center and co-author of the study, added that “the cyclic expansion can be induced by including light-responsive plasmonic nanoparticles embedded in the thermosensitive ink; this brings about changes in the hydration state of the temperature-sensitive polymer and thus in its volume; in other words, on-off stimulation takes place”. And by changing the composition of the thermosensitive polymer, they can effectively adjust the transition temperature and pulsatility of the artery.
A realistic alternative to traditional models for exploring therapeutic opportunities
Both stimuli-sensitive inks containing gold nanoparticles and cell-containing bioinks display properties suitable for printing in conjunction with highly porous structures, which facilitate the diffusion of nutrients, oxygen and heat throughout the system. More specifically, the inserting of gold nanoparticles into polymeric networks gives the system multifunctionality, and also enables a stimulus-response, because laser irradiation brings about a very localized increase in temperature without the cells becoming damaged, “since the physiological temperature is not exceeded”, added Jiménez de Aberasturi. “We have optimized the heating parameters to generate the expansion and contraction of the material using laser illumination, thus mimicking the pulsatility of arteries. The bioink is also biocompatible and provides a constructive environment for the growth of different types of cells,” Henriksen pointed out.
This novel approach to inducing pulsatile effects for building arterial models will allow a deeper understanding of molecular and cellular mechanisms to be gained, while providing a realistic alternative to traditional in vitro and in vivo models used to explore therapeutic opportunities. The researchers also stress that “there is a big variation in the geometric and physicomechanical properties of arteries in terms of species, tissue and health status of the artery in question”. They also added that “the use of these materials is not limited to arteries, but are of interest in the construction of any type of biomodel in which the biological effect of a physical change is to be studied”.