A study conducted by a team from the Spanish National Center for Cardiovascular Research (CNIC) in collaboration with a group from CIC biomaGUNE has found that mixing mitochondrial DNA (mtDNA) from two different origins may have detrimental effects in the long and medium term; mtDNA is part of the genetic material transmitted only from mothers to their offspring.
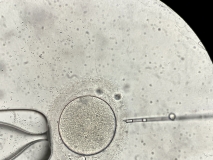
The work, published in Circulation, provides invaluable information when it comes to understanding and preventing the potential risks of therapeutic techniques involving mitochondrial transfer. The most popular among them are the techniques designed to improve fertility; they involve injecting mitochondria from a donor egg into the egg of a woman with fertility problems, or mitochondrial replacement, designed to prevent the transmission of pathological mutations to offspring, popularly known as "children of three genetic parents", and which has already been approved in the United Kingdom.
According to the study, although most cells rejected two mitochondrial variants and progressively eliminated one of the two mtDNAs, some organs, crucial ones such as the heart, lungs or skeletal muscle, were incapable of doing so.
For Dr José Antonio Enríquez, leader of the research and director of the Functional Genetics of the Oxidative Phosphorilation System (GENOXPHOS) laboratory at the CNIC, the information is especially relevant to the field of donor mitochondrial transfer therapies; this is because the work has shown that "animals that are apparently healthy in their juvenile stage suffered in the long term from heart failure, pulmonary hypertension, loss of muscle mass, frailty and premature death".
Most of the DNA in the cells of our body is organized in the nucleus of the cell. This is where the information for approximately 20,000 genes of the human genome is located. However, as Dr Enriquez explains, 37 genes are not located in the nucleus of cells: "they are located in cell subunits called mitochondria, where the mitochondrial DNA resides".
The DNA of the nucleus is transmitted from parents to offspring, with the mother contributing 50% and the father contributing the other 50%, and they combine in the fertilization of an egg by a sperm.
But mtDNA is only transmitted via the mother, since the sperm mitochondria are destroyed inside the fertilized egg. That is why mtDNA is said to be transmitted uniparentally in virtually all organisms. The mtDNA is also present in multiple copies in each cell, which are basically identical (a phenomenon known as homoplasmy).
The presence of more than one mtDNA variant in the same cell (heteroplasmy) can on rare occasions arise naturally due to mutations, and trigger various diseases, as the researchers explain. In this regard, in recent years various medical techniques aimed at preventing diseases and improving fertility have been proposed, and they can generate a new type of heteroplasmy, such as the popularly known "children of three genetic parents".
"The latter is called heteroplasmy between non-pathological mtDNA variants and involves combining the donor individual's mtDNA with that of the recipient. This means breaking one of the natural biological barriers that the GENOXPHOS group at the CNIC has investigated to clarify whether physiological alterations emerge in the individual," says Dr Enriquez.
The researchers reveal that the selection process between mtDNAs coexisting in the same cell depends on their impact on cell metabolism and can be modulated both by variations in the function of various genes and by the action of drugs or changes in the animals' diet. "All of these factors determine the preference for the selected type of mitochondrial genome," they write.
"The reason why nature has opted for mtDNA to be transmitted by only one parent raises an important biological question that has yet to be clarified but which until now has had no implications in the field of health," says Dr Ana Victoria Lechuga-Vieco, lead author of the article. "However, novel medical therapies can break this biological barrier and generate, by design or by accident, mixtures of mtDNA from more than one individual," warns this researcher.
In other words, until these data were published, "it was not known whether or not this mixture had repercussions for the individual," says Dr Enriquez, director of the research.
To answer this question, the GENOXPHOS group generated mice with identical nuclear DNA, while simultaneously possessing, in all their cells, mtDNA from two different individuals that differed from each other in terms of their genetic sequence. "This mouse lineage was fertile and did not display any pathology in the young animal," explains Dr Lechuga-Vieco.
However, as described in their research, analysis of these animals throughout their lives revealed that their mitochondrial function was impaired by the coexistence of two different mtDNAs in the same cell.
"We saw that the cells rejected the presence of two mitochondrial variants and most of them progressively eliminated one of the two mtDNAs. Surprisingly, organs as important as the heart, lung or skeletal muscle were unable to do so," explains Dr Lechuga-Vieco.
"The organs that were able to eliminate one of the two mtDNA variants, such as the liver, regained their mitochondrial metabolism and cell health, but those that failed to do so progressively deteriorated as the animals aged," stresses Dr Enriquez.
So the animals that appeared to be healthy in their juvenile stage suffered long-term "heart failure, pulmonary hypertension, loss of muscle mass, frailty and premature death", adds Jesús Ruíz-Cabello, Ikerbasque professor at CIC biomaGUNE and co-supervisor of Dr Lechuga-Vieco's PhD thesis.
The researchers conclude that the detrimental effects of these medical technologies observed in this study require careful selection of donor mtDNA for mitochondrial replacement therapies.
As they write in the article published in Circulation, even “the most promising method for the mitochondrial replacement of oocytes carrying known pathological mtDNA mutations can fail and 100% replacement may not be achieved."
The work further shows that recipient cells have a strong capacity to select and amplify pre-existing mtDNA, which may initially be undetectable, resulting in a potential mixture of mtDNA from two individuals. "The same problem arises when oocyte rejuvenation is performed by injection of donor cytoplasm," warns Dr Enriquez.
Likewise, adds the CNIC researcher, "a similar risk may arise with therapies that use purified mitochondria from a donor for damaged cells in the event of cardiopulmonary or neurological diseases".
However, these risks do not mean that mitochondrial replacement therapies should be dispensed with, stresses Dr Enriquez. Just as in blood transfusions or organ transplants where compatibility between donor and recipient must be monitored, Dr Enriquez recommends that any therapeutic strategy that may involve mixing healthy mitochondrial DNA from two individuals should "ensure mitochondrial genome compatibility between donor and recipient".
The research was conducted in collaboration with other research centers, including the biomaGUNE Cooperative Research Center, and has received support from the following funding bodies: Ministry of Economic Affairs and Digital Transformation (MINECO); Ministry of Economy, Industry and Competitiveness (MEIC);
Human Frontier Science Program; Guipuzcoa Science, Technology and Information Network Program of the Basque Government, and the Department of Industry, Innovation, Trade and Tourism of the ELKARTEK Program.