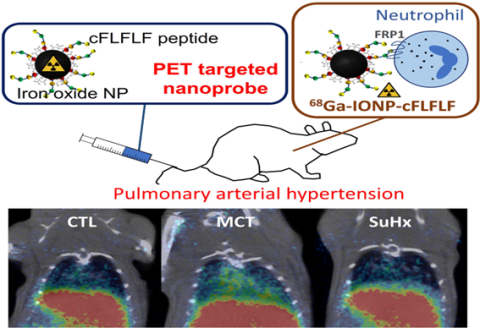
Pulmonary arterial hypertension (PAH) is a severe disease characterized by elevated blood pressure in the pulmonary artery that can ultimately damage the right ventricle of the heart. PAH is pathophysiologically heterogeneous, which makes early diagnosis and treatment difficult. Inflammation is thought to be an important factor in the development and progression of this disease and may explain some of the observed interindividual differences. In the context of both acute and chronic inflammation, neutrophil recruitment to the lung has been suggested as a potential biomarker for studying PAH progression. However, there are currently no specific probes for its non-invasive in vivo detection. The imaging-based gold standard for assessing inflammation is [18F] fluorodeoxyglucose (18F-FDG), which is not cell specific. This highlights the urgent need for more specific molecular probes to support personalized medicine.